Are You Drinking Enough Water? This Could Be Worsening Your Chronic Condition
Have you had been drinking water today?
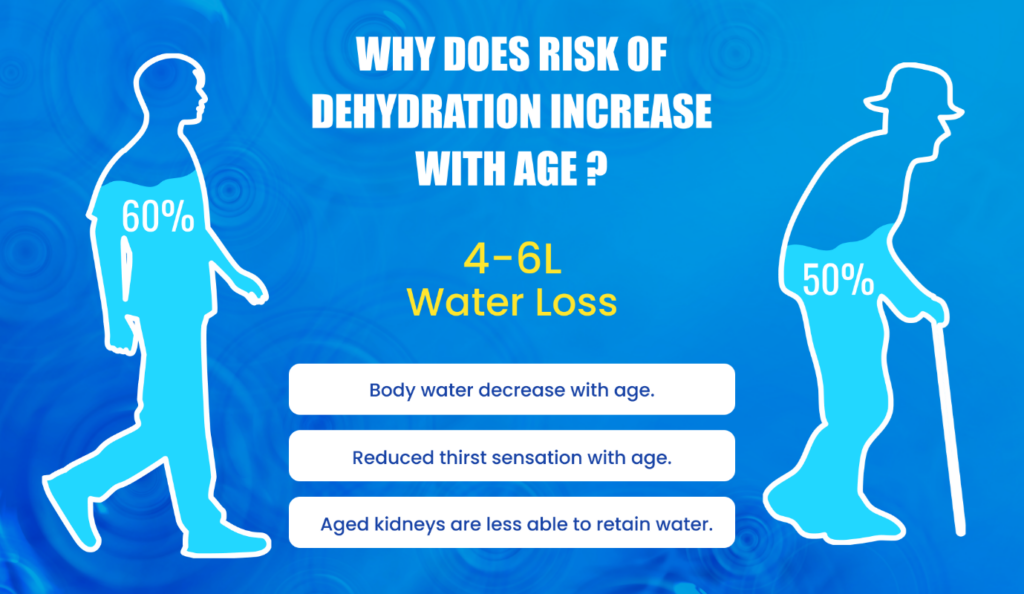
It’s a simple question, but for elderly individuals in our homes, the answer could be a matter of life and health. Studies show that dehydration affects 20% to 30% of the elderly population, with far more serious consequences than in younger individuals, leading to higher risks of illness, disability, and even life-threatening complications. Despite this, drinking water often gets overlooked, especially when managing chronic conditions like diabetes or arthritis. Let’s dive into why staying hydrated is such a game-changer for seniors and how it can make managing health much easier.
The importance of drinking water cannot be overstated, especially for seniors managing chronic conditions. Staying hydrated affects everything from kidney function to energy levels.
“Drinking Water: The Ultimate Fuel for Your Body”
Water is the unsung hero that keeps our bodies running smoothly. It plays a key role in regulating body temperature, ensuring we stay cool even on the hottest days. Water is also the main vehicle for transporting nutrients and oxygen to every cell, keeping our energy levels up and our organs functioning properly. Plus, water helps flush out waste, preventing toxins from building up, and keeps our joints well-lubricated, making movement easier and pain-free. Water is the ultimate fuel that powers every part of your body, from your cells to your joints. Are you giving your body the hydration it requires to keep running at its best?
“Hydration: Your Daily Dose of Wellness“
Dehydration can quietly worsen your chronic health problems. Take dementia, for example. Many older adults with cognitive decline struggle to drink enough water because they might forget, have trouble swallowing, or simply can’t express their thirst. This can lead to a vicious cycle where dehydration worsens their confusion and memory issues, making it even harder for them to stay hydrated.
Dementia can also result in seniors forgetting to follow their medication routine as prescribed by doctors. This is where you, as a caregiver can opt for a reliable
med reminder app like mySeniorCareHub can significantly improve medication adherence. This medication reminder app has a pill tracker feature that provides timely alerts and reminders, ensuring you never miss a dose.
Conditions like diabetes and kidney disease are also closely tied to hydration levels. Dehydration raises blood sodium levels, putting extra strain on the kidneys and making sugar management more difficult for diabetics. People with arthritis may find that dehydration exacerbates their joint stiffness and inflammation, making their condition worse. Dehydration has even been linked to obesity in older people because of altered fluid distribution, especially in women.
Table 1: Key Risk Factors for Dehydration in the Elderly
| Risk Factors | Explanation |
| Advanced Age (85+ years) | Natural changes in the body increases the risk of dehydration as people age. |
| Reduced Thirst | Aging reduces the sensation of thirst, making it harder to recognize the need to drink. |
| Difficulty Accessing Drinks | Mobility or physical challenges can limit their ability to get water. |
| Communication Barriers | Challenges in expressing the need for water, especially in speech-impaired individuals. |
| Cognitive Disorders | Conditions like dementia may prevent recognizing or communicating thirst. |
| Swallowing Problems | Difficulty swallowing (dysphagia) can reduce fluid intake. |
| Loss of Appetite | Eating less often leads to lower fluid intake, as many foods provide water. |
| Medications | Drugs like diuretics, laxatives, or sedatives can increase fluid loss. |
| Illnesses | Acute issues like fever, vomiting, or diarrhea can deplete body fluids quickly. |
| Caregiver Oversight | Lack of attention to hydration needs can worsen the risk. |
The message is simple: staying hydrated can make a world of difference. So, could drinking more water be the small change that helps you feel better every day?
Signs of Dehydration and Their Misinterpretation
Now that we’ve explored how dehydration can affect chronic conditions, let’s talk about spotting the warning signs—especially in elderly loved ones. How do you know if they’re just tired or if it’s something more serious? Dehydration can be sneaky, showing up as dry mouth, fatigue, sunken eyes, or muscle cramps. Noticed darker urine or fewer bathroom trips? That’s a red flag, too. But here’s the tricky part: these signs often get brushed off as part of aging or blamed on other health conditions like diabetes or arthritis.
Things get even more serious with symptoms like a racing heart, confusion, fainting, or diarrhoea and vomiting that stick around. Ignoring these can lead to complications such as kidney issues, seizures, or even heat exhaustion. Caregivers, this is your cue: watch for these subtle but important signals. Could dehydration be hiding in plain sight in your home? It’s time to make hydration a habit, not an afterthought.
Hydration Strategies for Chronic Condition Management
Let’s get practical—how can we keep hydration on track? The golden rule: drink regularly, even if you’re not thirsty. Aging reduces thirst cues, so it’s important to sip water throughout the day, just like athletes hydrate as a routine, not only when parched. Aim for at least 1.7 L of fluids daily. Hydration doesn’t have to mean plain water. Tea, fruit juices, milk, soups, and water-rich foods like fruits, vegetables, fresh cheese, and yogurt are great options. Small, frequent sips are better than large gulps, as drinking too much at once can reduce thirst further.
Table 2: Simple Steps to Prevent Dehydration in the Elderly
| Steps | Description |
| Educating Caregivers and Healthcare Staff | Provides easy-to-understand hydration tips and strategies for those caring for the elderly. |
| Encourage Drinking Regularly | Teach elderly individuals to drink water even when they’re not feeling thirsty. |
| Spot High-Risk Individuals | Identify elderly people who might be more prone to dehydration, such as those with chronic illnesses. |
| Ensure Easy Access to Drinks | Keep water and other fluids within easy reach, especially for those with mobility challenges. |
| Promoting Healthy Drinking Habits | Remind and encourage elderly individuals to sip fluids throughout the day. |
| Review Medications | Keeping an eye on any prescribed medication that could increase the risk of dehydration. |
| Monitor Appetite | Watch for signs of poor appetite, which can affect fluid intake. |
| Removing Environmental Barriers | Address factors like hard-to-use water bottles or lack of nearby drinking options. |
Take the Hydration Pledge: Sip Your Way to Better Health!
By using an app for tracking medications like mySeniorCareHub into your daily routine, you can streamline your healthcare management and ensure you’re achieving your hydration goals and following medication schedules. Keep in mind that drinking only a glass of water can have a profound impact on your health. To make hydration a seamless part of daily life, use a meds reminder like mySeniorCareHub mobile application. Enable push notifications on your Android or iOS device and set reminders to drink water at regular intervals, ensuring you stay consistent and hydrated without having to rely solely on memory. With a little effort and the right strategies, staying hydrated can become a habit that empowers you to lead a healthier, more comfortable life. So, take that first sip—it’s never too late to start!









