How to Prevent Medication Overdose in Older Adults
Medication Overdose is one of the biggest concern among patients
“Did I already take my pill… or not?”
This was the third time in a week that 78-year-old Nancy had asked the same question.
Nancy lives in Ohio, and like many older adults, she values her independence. Her daughter, Emma, visits every weekend. One Saturday, Nancy mentioned feeling dizzy and had trouble keeping her balance. Emma checked the medicine cabinet and noticed two pills of the same kind had been taken for the day instead of one. That same evening, they ended up in the ER. Diagnosis? Accidental overdose.
This kind of situation is way more common than you might think. And it doesn’t just happen to people living alone. Overdose in seniors is a quiet but dangerous problem. One that stems from forgetfulness, multiple medications, and a lack of timely support.
Let’s talk about why it happens, how to catch the signs early, and how using tools like mySeniorCareHub can keep our loved ones safe.
Medication Overdose – Why Does This Happen So Often?
As people get older, their bodies and brains change. That’s natural. But that also means managing medications becomes harder. Here are a few reasons why overdoses happen:
● Memory slips (especially in dementia) – It’s easy to forget if you took your meds already. Conditions like Alzheimer’s or mild cognitive impairment make it worse.
● Too many prescriptions (called “polypharmacy”) – Most seniors take 5 or more pills a day. That’s a lot to keep track of! One missed dose or extra pill can throw things off.
● Vision problems – Tiny print on bottles. Similar-looking pills. It’s a recipe for mix-ups, especially in low light.
● Shaky hands, arthritis, or poor grip – For someone with mobility issues, it can be difficult to cut tablets in half and open bottles.Changes in the body with age – The liver and kidneys slow down with age. That means the body clears drugs more slowly, and even small overdoses can become toxic.
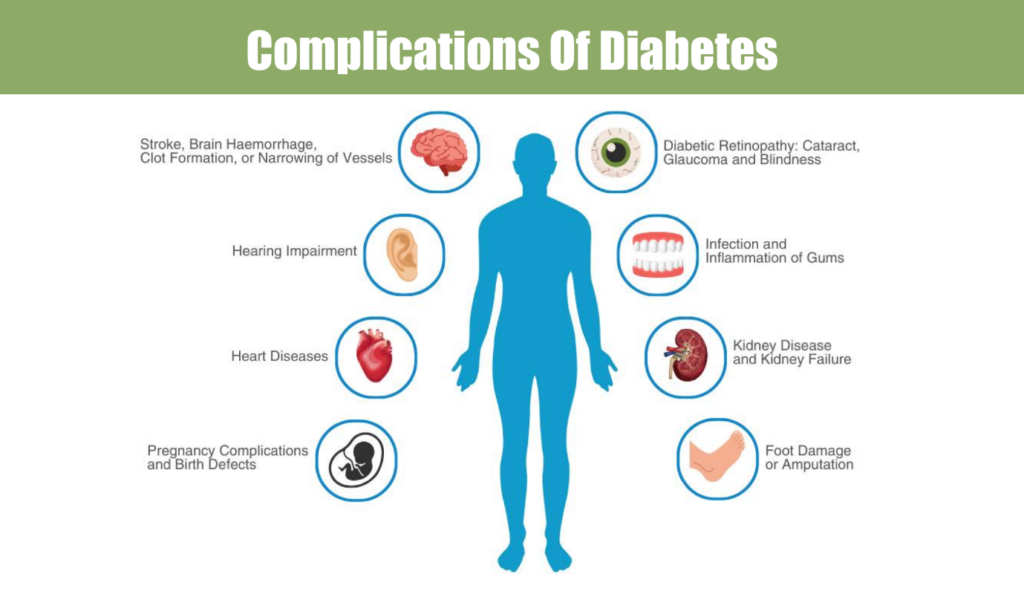
Some Medications Are Riskier Than Others – Avoid Medication Overdose
Here are some of the most common drugs involved in senior overdoses:
| Drug Type | Examples | What Can Go Wrong |
| Blood thinners | Warfarin, Xarelto | Easy bruising, internal bleeding |
| Diabetes meds | Insulin, Glipizide | Low blood sugar, confusion |
| Sleeping pills | Ambien, Diazepam | Drowsiness, falls, slow breathing |
| Painkillers | Oxycodone, Tramadol | Trouble breathing, sedation |
| Heart meds | Metoprolol, Lisinopril | Low blood pressure, fainting |
Warning Signs in Overdose – Important Information of Medication Overdose
Sometimes, the signs of overdose in seniors are subtle. And sadly, they’re often blamed on “just getting old.”
Watch out for:
- Extreme tiredness or sleeping too much
- Confusion or acting “off”
- Slurred speech or slow movements
- Nausea or vomiting
- Unsteady walking or more frequent falls
- Trouble breathing
If something feels wrong, trust your gut. Better safe than sorry.
How mySeniorCareHub Can Help – App for Solving Medication Overdose
This app was created with care and with seniors in mind. It is not about introducing more technology into their lives. It is about making everyday tasks easier and safer.
Here’s how:
Gentle medication reminders
- Pops up when it’s time to take a pill.
- Easy tap to mark it as ‘taken.’
Keeps caregivers in the loop
- If Grandma skips a dose or takes two, her daughter gets a ping.
- It is also possible to connect with a nurse or senior care companion.
Medication history at a glance
- Helpful for doctor visits.
- Tracks patterns: “Are they skipping night meds?”
Tracks cognitive health
- Picks up on increasing forgetfulness.
- It can even indicate whether memory issues are worsening.
Emergency alerts
- If a senior has a sudden drop in blood pressure or other unusual vital signs, an alert is sent.
- GPS helps emergency teams locate them fast.
Other Simple Fixes That Work
Technology is amazing, but even small daily changes can help avoid overdose:
✔ Use weekly pill organizers
Simple, labelled containers can reduce mistakes. Some even beep!
✔ Get regular “med checks.”
Ask your doctor or pharmacist to review all meds. You’d be surprised how many can be reduced or stopped.
✔ Use voice reminders
Especially in their voice or a loved one’s voice. Makes it feel more personal.
✔ Talk openly
Create a routine: “After breakfast, let’s take meds together.”
✔ Colour-code bottles
The sticker system can help red = morning, blue = evening.
Let’s Be Real for a Second…
No one wants to feel like they’re being watched. Seniors want their dignity, not babysitting. The beauty of mySeniorCareHub is that it helps quietly in the background.
It supports independence. It provides safety without intruding.
And most importantly, it brings peace of mind to families who can’t always be there in person.
When to Call 911
If your loved one:
- Is passed out or extremely drowsy
- Has trouble breathing
- Is confused or hallucinating
- Has seizures or chest pain
Call for help immediately. Bring any pill bottles or a list of medications with you.
Final Words from the Heart
We all want our parents and grandparents to live with dignity, comfort, and safety. But accidental overdoses can take that away in an instant.
Let’s be proactive & Use Best Medication App
Because managing meds shouldn’t be a daily stress. With the right support, it can just be part of a healthy routine.
mySeniorCareHub is more than an app. It’s a promise that someone is always watching out for the people you love.
Let’s make senior years safer, together.
Download mySeniorCareHub and help your loved ones stay on track, stay safe, and stay independent.