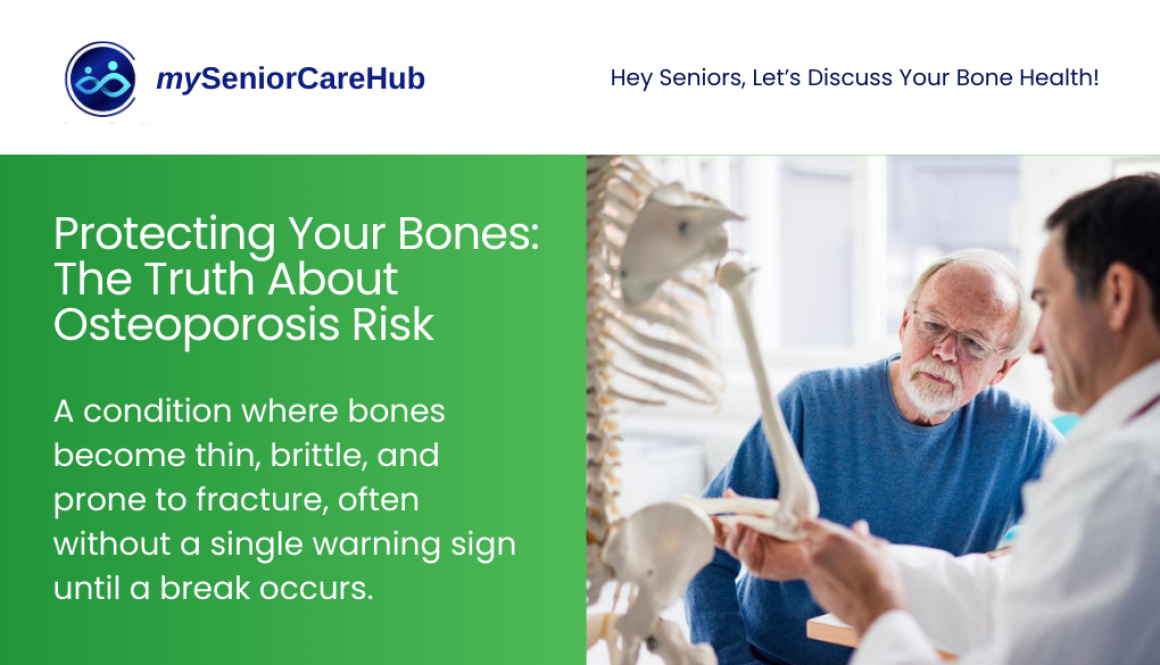
Could You be at Risk for Osteoporosis? Let’s Talk About It!
As we move into 2026, bone health has become a front-and-center priority for healthy aging. Often called the “silent thief,” osteoporosis is a condition where bones become thin, brittle, and prone to fracture, often without a single warning sign until a break occurs.
If you are over the age of 60, understanding your risk isn’t just about “getting older”; it’s about protecting your independence. Here is the latest data and medical guidance to help you stay strong and mobile.
The Alarming Reality: 2025–2026 Statistics
Recent global health reports from late 2025 highlight a growing crisis in bone health. As our population ages, the “bone gap,” the difference between those at risk and those receiving treatment, continues to widen.
- The 1-in-3 Rule: Current data confirms that 1 in 3 women and 1 in 5 men over the age of 50 will experience an osteoporotic fracture in their lifetime.
- The Diagnostic Gap: Shockingly, up to 80% of seniors who suffer a first fracture are never formally diagnosed or treated for the underlying osteoporosis, leaving them at extreme risk for a second, more debilitating break.
- The 2050 Projection: Experts predict that hip fractures will nearly double by 2050 if current screening rates do not improve.
Are You at High Risk? (The 2026 Checklist)
While age is the primary factor, several specific indicators can tell you if you need to schedule a bone density scan (DEXA) immediately:
- Height Loss: Have you lost more than 1.5 inches (4 cm) from your peak adult height? This is often the first sign of “silent” vertebral fractures.
- Fragility Break: If you broke a bone from a simple trip or a fall from standing height, it is medically considered an osteoporotic fracture until proven otherwise.
- Family History: If either of your parents suffered a hip fracture, your genetic risk is significantly higher.
- Medication Use: Long-term use of steroids (prednisone), certain antidepressants, or even some heartburn medications (PPIs) can leach calcium from your bones.
- Body Frame: Individuals with a BMI below 19 or a very small, thin frame have less “bone bank” to draw from as they age.
New Screening & Treatment Standards for 2026
Medical guidelines updated for 2026 have shifted toward proactive intervention.
1. Precision Screening
The U.S. Preventive Services Task Force and other global bodies now recommend:
- Universal screening for all women aged 65+.
- Clinical Risk Assessment for postmenopausal women under 65 and men over 70.
- Earlier Screening if you have “secondary” risk factors like Rheumatoid Arthritis or Type 2 Diabetes.
2. Advanced Treatment Options
If you are diagnosed with Osteoporosis, 2026 brings more options than ever. Beyond the standard weekly pill (bisphosphonates), new Anabolic (Bone-Building) Agents like Romosozumab and Teriparatide are now being used earlier for high-risk patients to actively rebuild bone density rather than just slowing its loss.
Your 2026 Bone Protection Plan
You are never too old to start “saving” your bone mass. Here is how to take action today:
- Prioritize Protein & Calcium: Aim for 1,200 mg of calcium daily, preferably from food (yogurt, sardines, leafy greens). Protein is equally vital for the “collagen” matrix of your bones.
- The Vitamin D Update: 2025 studies suggest that while supplements are common, 800–1,000 IU is the “sweet spot” for seniors, especially those with limited sun exposure.
- Resistance Training: Walking is great, but weight-bearing exercise (like lifting light weights or using resistance bands) is what actually signals your bones to stay strong.
- Fall-Proof Your Life: Most fractures happen at home. Remove throw rugs, install grab bars in the bathroom, and brighten your home’s lighting.
The Bottom Line is that Osteoporosis is preventable and treatable, but only if you know your status. Don’t wait for a fracture to find out where you stand.